
Onychomycosis, or, as it is popularly called, nail fungus, is damage to the nail plate and adjacent structures by a fungal infection. Nails infected with fungus change color and transparency, become brittle, rough, thickened, peel and crumble. In this case, the tissue beneath or near the nail may become red and swollen.
Nail fungus is a very common condition. According to statistics, onychomycosis affects from 8 to 26. 9% of the world's population, and in Russia the number of people with this diagnosis ranges from 4. 5 to 15 million people.
Typically, onychomycosis is found in patients over 40 years of age. At the same time, there are no uniform statistics on the frequency of occurrence of the disease in men and women, the authors' opinions differ. In Russia, nail fungus is more common in men. At the same time, women are one and a half times more likely to consult a doctor - perhaps this is explained by a more attentive attitude to the health and appearance of their finger and toe nails. The photos may seem shocking.

In approximately 80% of cases, the disease affects the toenails. Less commonly, onychomycosis affects the nails. Researchers have identified factors that significantly increase the risk of developing onychomycosis. They can be roughly divided into two groups.
External (exogenous) risk factors for the development of onychomycosis:
- nail injuries;
- prolonged use of tight, non-breathable shoes;
- stay in a hot, humid climate.
Internal (endogenous) risk factors for the development of onychomycosis:
- patient's age: the disease is more common in people over 40 years old;
- overweight;
- decreased immunity;
- associated diseases: diabetes mellitus, thyroid disease, varicose veins;
- flat feet and other foot deformities;
- prolonged use of certain medications: antibiotics, cytostatics, corticosteroids.
The family factor plays a special role in the spread of onychomycosis. According to statistics, 55% of patients had a family history of nail fungus.
You can become infected with onychomycosis through direct contact with an infected person, as well as through household items - clothes, shoes, hygiene products (rags, towels).
In public places, infection occurs mainly in gyms, baths, saunas and swimming pools. Scales with pathogenic fungi end up on floors, benches, paths and railings. Fungi in these conditions continue to multiply and soon find new hosts.

The fungi that cause onychomycosis reproduce well in conditions of high humidity. Also, you can catch onychomycosis in a manicure or pedicure salon if the master does not follow the rules of hygiene and sterilization of instruments.
Causes of onychomycosis
Around 50 species of fungi are known that can infect the nail plate. At the same time, dermatomycetes of the genus Trichophyton are responsible for up to 80-90% of cases of onychomycosis of the feet and up to 36% of onychomycosis of the hands.
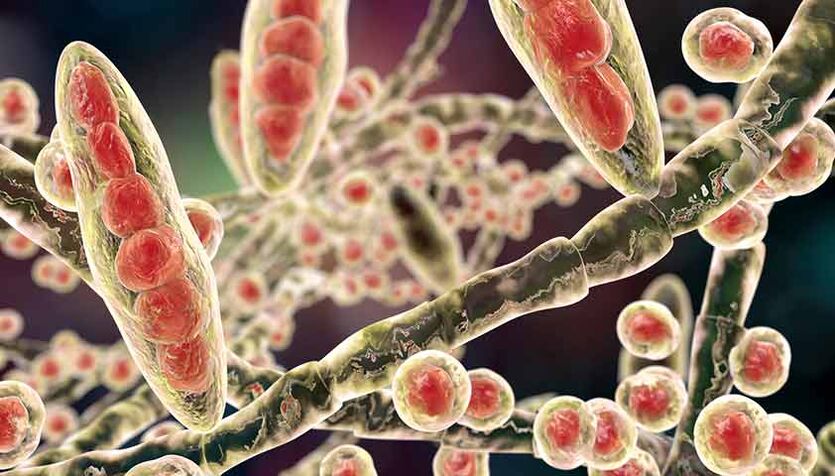
Dermatomycetes are microscopic fungi that attack the skin, hair and nails. The second most common causative agents of onychomycosis are yeasts of the genus Candida (candida). Nail candidiasis occurs in 5–10% of cases. The least common causative agents of onychomycosis are mold fungi - Aspergillus (Aspergillus), Fusarium (Fusarium), Scopulariopsis (Spoculariopsis).
In practice, the nail plate is damaged by several types of fungi at the same time. Most often it is a combination of two types of dermatomycetes or variations of "dermatomycetes + yeast", "dermatomycetes + mold". In approximately 10% of cases, the patient is infected with three or more types of fungi.
Types of onychomycosis
In Russian dermatology, three types of onychomycosis are distinguished, depending on the clinical manifestations of the disease.
Main types of onychomycosis:
- normotrophic: the shape of the nail plate does not change, while whitish and yellowish stripes are visible in the thickness of the nail;
- hypertrophic: the nail plate visibly thickens, becomes brittle, with uneven edges;
- dystrophic: the nail plate becomes thinner and becomes detached from the nail bed.

Depending on how the fungus got into the skin and nails, there are four types of onychomycosis.
Types of onychomycosis depending on the place of penetration and spread of the pathogenic fungus on the nail plate:
- superficial white: the fungus colonizes the upper part of the nail plate. Whitish lesions appear on the nail. As the infection spreads, the nail turns gray-brown and begins to crumble;
- distal-lateral subungual: the fungus penetrates the skin in the region of the nail folds or the free edge of the nail. The nail plate thickens, turns yellow, collapses and then moves away from the nail bed;
- proximal subungual: the fungus spreads from the skin and nail folds to the nail plate and deeper. Spots appear on the nail in the hole area and on the nail bed. The nail plate comes off;
- total dystrophic: the entire nail plate is affected. It appears quite thickened and turns a dirty yellow color. The surface of the nail becomes uneven.
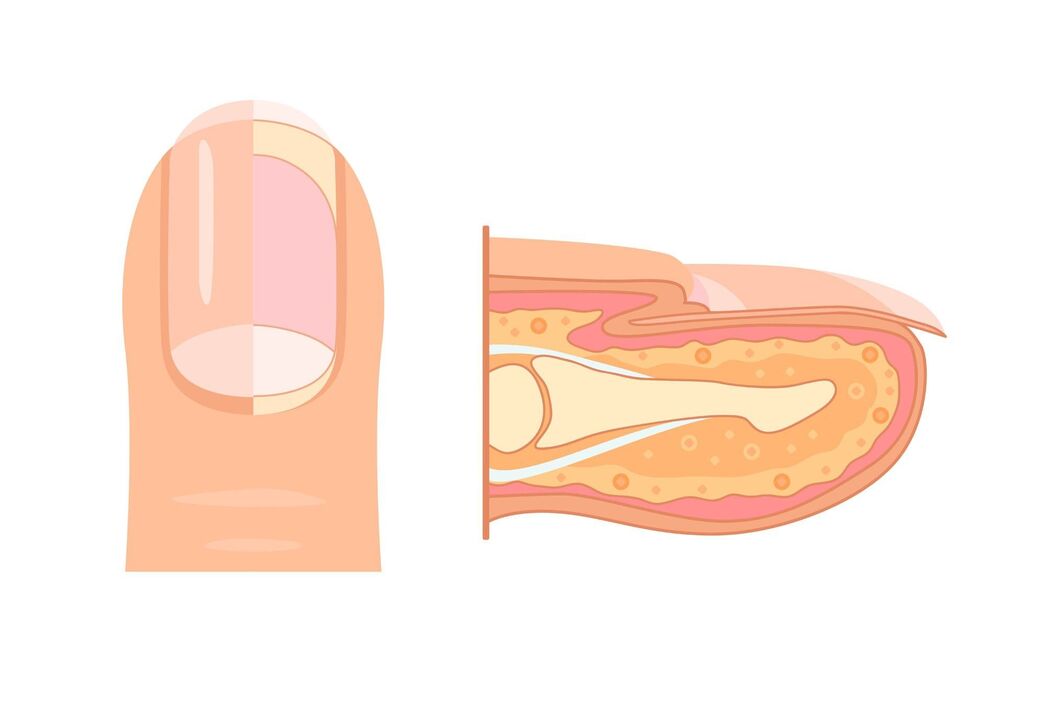
Once on the nail plate or surrounding structures, the fungal colony begins to grow towards the matrix - the growth zone, located at the back of the nail bed. It is believed that the faster the nail grows, the more effectively it displaces the fungal colony and the sooner recovery from onychomycosis occurs. This mechanism also explains the fact that nail fungus mainly affects people over 40: their nails grow much more slowly than those of young people.
Symptoms of onychomycosis
As onychomycosis progresses, the symptoms of the disease become more pronounced.
The main symptoms of onychomycosis:
- change in the color of the nail plate to yellow, black, green, brown or gray;
- separation of the nail plate from the bed;
- change in the thickness of the nail plate;
- koilonychia - the nail is concave, shaped like a teaspoon;
- onychogryphosis - the nail bends like the beak of a bird of prey;
- thickening of the nail bed;
- change in the surface of the nail plate: formation of pits, furrows, furrows;
- inflammation of the nail fold.
Complications of onychomycosis
Without treatment, onychomycosis in patients with diabetes can lead to serious complications such as diabetic foot - ulcerative soft tissue defects with damage to tendons and bone structures.

In people with long-term fungal infection, as well as in a context of immunodeficiency, onychomycosis can lead to a severe allergic reaction. This is explained by the fact that the fungal colony and its metabolic products act as sensitizers - triggers to which the body reacts with greater sensitivity.
As a result, an allergic reaction is formed, which can have different manifestations: a more severe course of bronchial asthma, the appearance of foci of microbial eczema and the development of urticaria.
Common complications of onychomycosis:
- diabetic foot;
- Allergic reactions;
- chronic erysipelas of the extremities is an infectious lesion of the skin;
- lymphostasis - retention of lymphatic fluid in tissues;
- elephantiasis (elephantiasis, elephantiasis) is a progressive lymphatic edema simultaneously with the replacement of subcutaneous adipose tissue with connective tissue.
Diagnosis of onychomycosis
The diagnosis and treatment of onychomycosis are made by a dermatologist. During the consultation, the doctor will assess the condition of the patient's nails, skin, mucous membranes and hair. He will perform a dermoscopy and examine the enlarged skin. At the same time as the examination, the specialist will take an anamnesis and ask the patient about their lifestyle, quality of diet, domestic habits and care. If you suspect onychomycosis, your doctor will order laboratory tests. Examination of nail plate scrapings will rule out or confirm a fungal infection. The doctor may also refer the patient for microscopic examination and culture.
Diabetes mellitus can significantly worsen the course of onychomycosis and lead to serious complications. Complex studies can exclude or confirm this diagnosis. A complete blood count helps assess the patient's general condition.
Treatment of onychomycosis
Treatment of onychomycosis can be local, systemic or combined. Corrective therapy may also be required, which is aimed at eliminating concomitant diseases. In local therapy, antifungal medications are applied directly to the nail plate and nail folds. In this case, the medicine is concentrated on the surface of the nail and does not penetrate the bloodstream, eliminating the risk of side effects.
However, with local therapy, the medicine cannot always reach the fungal colony, especially if it is located deep in the nail bed. Before applying topical medications, the affected part of the nail must be removed. At home, you can use a keratolytic patch - it contains a small amount of acid and can soften the nail.
Systemic therapy allows the antifungal agent to penetrate the affected area through the blood, regardless of the depth of the fungal colony.
The main types of systemic drugs for the treatment of onychomycosis:
- antifungal agents;
- antiseptics - have antifungal and antibacterial effects;
- Multicomponent medicines may also contain anti-inflammatory substances.
The treatment regimen and dosage of the drug are determined by the doctor. In combination therapy, systemic and local treatment are carried out simultaneously. This makes it possible to increase the effectiveness of the treatment and reduce its duration.
Corrective therapy aims to treat concomitant diseases that can complicate the course of onychomycosis. These are mainly diabetes mellitus, thyroid pathologies and vascular diseases (e. g. varicose veins). Treatment tactics are determined by the doctor and other specialized specialists, who in this case take care of the patient together.
Forecasting and prevention
If you consult a doctor in a timely manner, the prognosis for onychomycosis is favorable: up to 80% of patients treated with antifungal drugs get rid of the disease forever. To prevent onychomycosis, it is necessary to protect the feet and hands from irritating and traumatic factors and strengthen the immune system.
Measures to prevent onychomycosis:
- change socks every day or more often if your feet are sweaty or wet;
- airy or dry shoes after use;
- do not use shared slippers during the visit;
- do not try on shoes in a store barefoot;
- use a personal towel for your feet;
- use individual tools for nail care (tweezers, files);
- wear shoes in the pool or sauna;
- monitor the diversity of your diet;
- avoid stressful situations.























